WHAT WE DO
At AQVerify, we are dedicated to revolutionizing the medical billing industry through our online portal. Our portal is meticulously made to empower medical billing companies of all sizes, offering a best features tailored to optimize efficiency and enhance revenue.

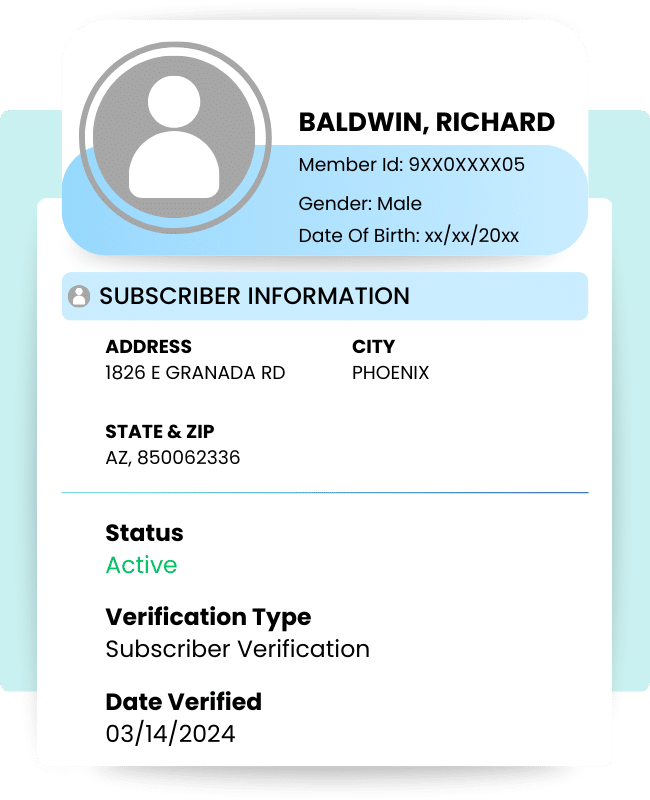
Eligibility Verification
Streamline the verification process with our advanced eligibility verification feature. It gives accurate patient coverage details, reducing claim rejections and minimizing revenue loss.

Claim Status Check
Track the status of claims effortlessly with our claim status check feature. Gain real-time insights into claim processing, allowing for proactive management and resolution of issues.

Same Or Similar
Simplify the identification of same or similar services with our specialized functionality. Enhance compliance and reduce claim denials by identifying duplicate within the billing system.
OUR PRODUCt
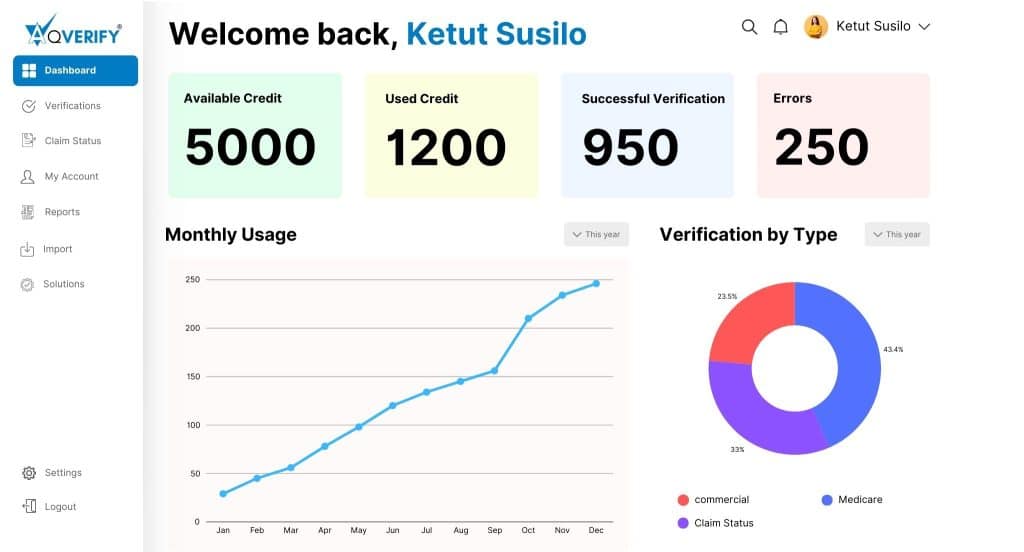
Get the most out of our online portal
Eligibility Verification
Get Accurate Patient Coverage Details
- Real-Time Verification
- Seamless Integration
- Customizable Criteria
- Comprehensive Reporting
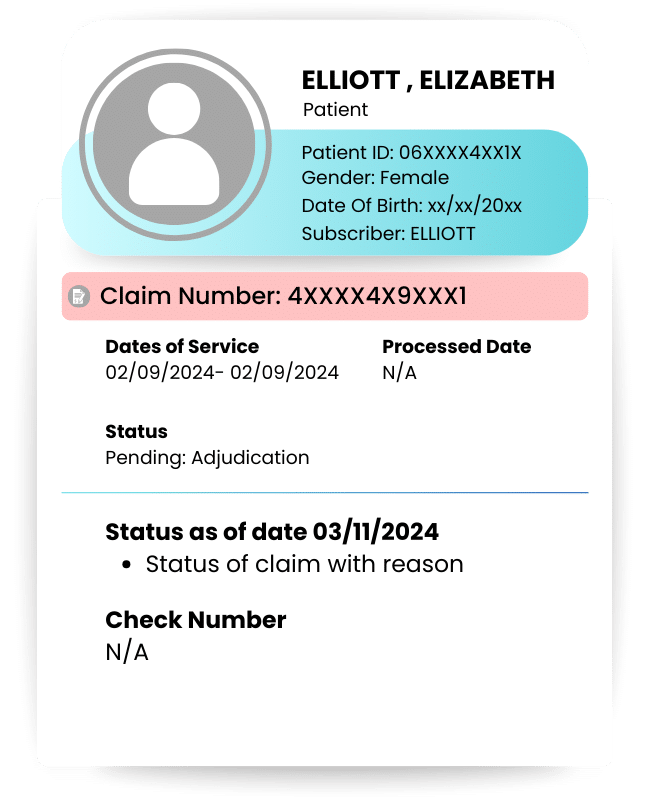
Stay Informed Every Step of the Way
Effortless Claim Status Tracking
- Real-Time Updates
- User-Friendly Interface
- Claim Status Automated Notifications
- Dedicated Support
Why choose AQVerify?
AQVerify’s innovative technology-based solution provides you with complete provisional information in a home-style spreadsheet, which helps you to get the best eligibility solution to increase the potency in the administration.
AQVerify helps you to provide all types of payers, including Medicare, Medicaid, BCBS, and commercial all across the United States. Our unalloyed process helps your administration to collect applicable patient payments and points inappropriate insurance data or patient demographics information.
TESTIMONIALS
No matter which service you select, rest assured that our dedicated team of experts is committed to delivering unparalleled support, ensuring you harness the full potential of our portal.